How to Recognize Signs of an Ear Infection sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality from the outset.
Ear infections are common ailments that affect individuals of all ages, yet their signs and symptoms can often be overlooked. Understanding the various types of ear infections, their causes, and how to identify them is essential for timely intervention. This guide aims to illuminate the key indicators that suggest the presence of an ear infection, empowering readers with the knowledge to seek appropriate care and treatment.
Understanding Ear Infections
Ear infections, medically known as otitis media, are common conditions that can affect individuals of all ages, particularly children. They occur when the middle ear becomes inflamed or infected, often resulting from various underlying factors. Recognizing the signs and symptoms of these infections can lead to prompt treatment and prevent potential complications.
Ear infections can be categorized into several types, each with distinct characteristics and causes. The three main types include acute otitis media, which is a sudden onset infection characterized by significant pain and fever; otitis media with effusion, where fluid builds up in the middle ear without symptoms of infection; and chronic otitis media, which is a long-lasting infection that can cause persistent ear problems.
Understanding these categories is crucial for effective management and treatment.
Common Causes of Ear Infections
Several factors contribute to the development of ear infections, and understanding these can help in prevention and early intervention. The following are common causes:
- Upper Respiratory Infections: Conditions such as colds and sinus infections can lead to inflammation and fluid accumulation in the ear.
- Allergies: Allergic reactions can cause swelling in the nasal passages and Eustachian tubes, obstructing airflow and fluid drainage.
- Environmental Factors: Exposure to cigarette smoke or pollutants can irritate the ear and respiratory tract, increasing infection risk.
- Anatomical Factors: Some individuals, especially children, may have shorter or more horizontal Eustachian tubes, making them more susceptible to infections.
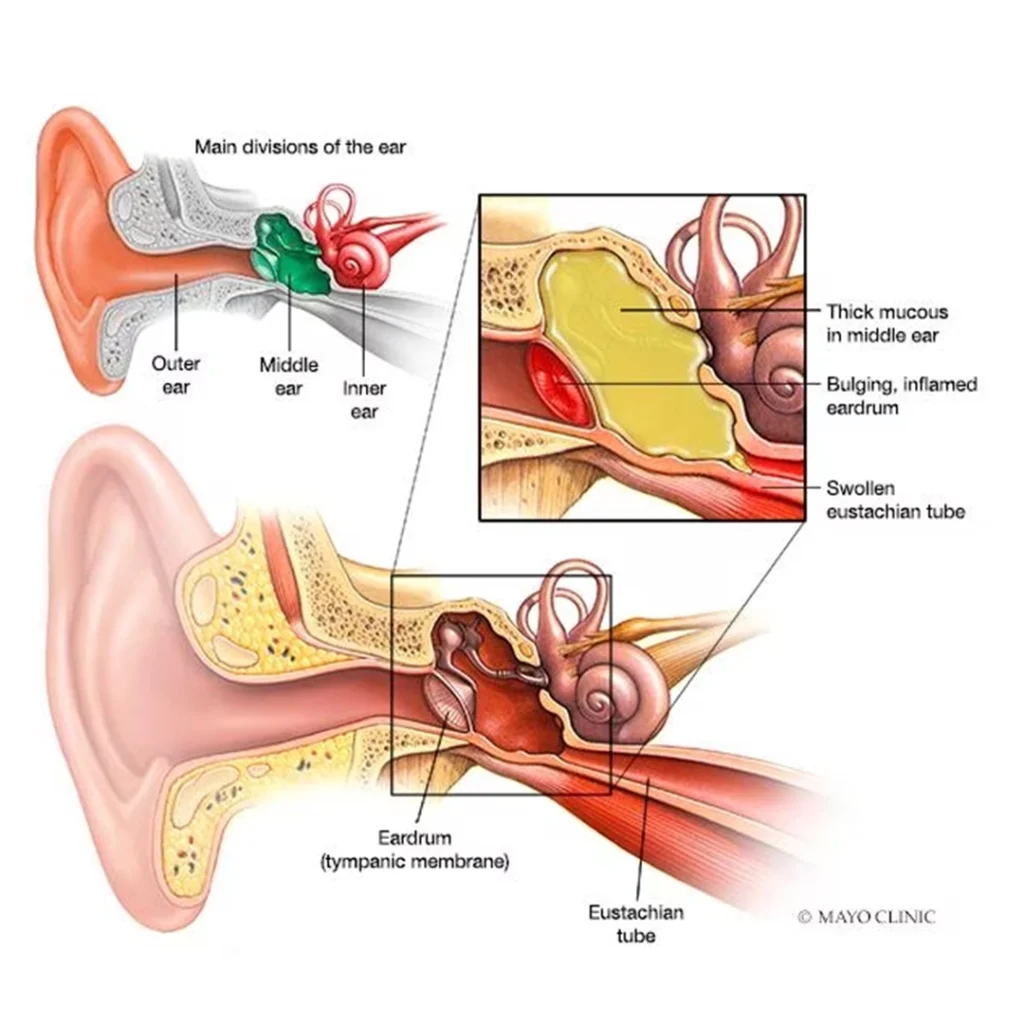
Anatomy of the Ear Related to Infections
Understanding the ear’s anatomy is essential when discussing infections. The ear consists of three main parts: the outer ear, the middle ear, and the inner ear. The middle ear, located behind the eardrum, contains small bones that transmit sound vibrations. It is connected to the throat through the Eustachian tube, which helps maintain equal pressure on both sides of the eardrum.
Infections typically occur when bacteria or viruses invade the middle ear, often following an upper respiratory infection. The Eustachian tube’s dysfunction can lead to fluid accumulation, creating an ideal environment for bacterial growth. This can result in symptoms such as ear pain, fever, and irritability in children.
Understanding the link between the anatomy of the ear and the mechanisms of infection is crucial for effective diagnosis and treatment.
Signs and Symptoms of Ear Infections
Recognizing the signs and symptoms of an ear infection is crucial for timely treatment and recovery. Ear infections can lead to discomfort and potential complications if left untreated. Understanding both common and less common symptoms is essential for identifying the condition early, particularly in vulnerable populations such as children and the elderly.Common signs indicating an ear infection typically manifest through various physical symptoms.
These can significantly affect daily activities and quality of life. The following list Artikels the most prevalent indicators of an ear infection:
- Ear Pain: Often described as a sharp, stabbing sensation or a dull ache, ear pain is the most recognizable symptom. It may worsen when lying down due to increased pressure in the ear.
- Trouble Hearing: An ear infection can lead to fluid buildup, which may cause a temporary reduction in hearing capacity.
- Fever: A mild to moderate fever may occur as the body responds to the infection.
- Fluid Drainage: Pus or fluid may drain from the ear, indicating a more severe infection or ruptured eardrum.
- Irritability and Fussiness in Children: Young children may express discomfort through increased irritability and difficulty in sleeping.
Less common symptoms may also suggest an ear infection, particularly in specific demographics. These symptoms can include:
- Dizziness or Balance Issues: Infections affecting the inner ear can lead to feelings of dizziness or loss of balance.
- Nausea or Vomiting: Some individuals may experience nausea or vomiting in conjunction with ear infections.
- Headaches: Persistent headaches can accompany ear infections, often due to related sinus pressure or tension.
The presentation of symptoms can differ notably between adults and children. Adults are more likely to report specific symptoms, such as ear pain and hearing difficulties, while children may show a broader range of reactions, including increased fussiness and changes in behavior. Children may also be more susceptible to recurrent ear infections due to anatomical differences in their ear structure, leading to a higher incidence of fluid accumulation.
In contrast, adults might experience complications less frequently but may have more severe pain and hearing loss when infections occur.
Understanding the varied symptoms of ear infections is essential for effective diagnosis and treatment, ensuring better health outcomes.
Risk Factors for Ear Infections
Ear infections are a common health issue affecting individuals of all ages, but certain demographic and environmental factors can increase the likelihood of their occurrence. Understanding these risk factors is essential for prevention and timely intervention.Demographic factors play a significant role in the susceptibility to ear infections. Certain groups are more commonly affected, particularly children. The anatomy of children’s ears, including a shorter Eustachian tube, makes it easier for bacteria and viruses to reach the middle ear.
Additionally, age is a crucial factor; children between six months and two years are at the highest risk due to their developing immune systems. Furthermore, gender influences susceptibility, as boys are generally more prone to ear infections than girls.
Environmental Factors Contributing to Ear Infections
Environmental factors significantly influence the prevalence of ear infections. Various conditions in one’s surroundings can increase the risk of developing these infections. Exposure to smoke, especially tobacco smoke, is particularly harmful, as it can irritate the respiratory tract and Eustachian tubes, leading to blockages. Crowded living conditions also heighten the risk, especially in daycare settings where children are in close contact with one another.
Seasonal changes can affect the incidence of ear infections, particularly during cold and flu season when respiratory infections are more common. All of these factors contribute to a higher likelihood of bacteria and viruses entering the ear canal.
Allergies and Respiratory Infections Related to Ear Infections
Allergies and respiratory infections are closely associated with ear infections, as they can lead to inflammation and blockage of the Eustachian tube. Allergies, such as those to pollen or dust mites, can cause nasal congestion and fluid build-up in the middle ear, increasing the risk of infection. Respiratory infections, including the common cold and sinusitis, often precede ear infections. When a respiratory infection occurs, the mucous membranes become inflamed, causing increased mucus production, which can obstruct the Eustachian tubes.
This obstruction prevents proper drainage of fluid from the middle ear, creating an environment conducive to bacterial growth.
“Understanding the interplay between allergies, respiratory infections, and ear infections is vital for effective prevention strategies.”
Diagnosis of Ear Infections
:max_bytes(150000):strip_icc()/GettyImages-1435293496-cf6df0709b6b490cb74d02de3b6d9cb8.jpg)
The diagnosis of ear infections is a critical step in ensuring appropriate treatment and management. Healthcare professionals utilize various methods to accurately identify the presence of an ear infection, which can significantly impact a patient’s overall health and quality of life.Otoscopy is a fundamental tool in diagnosing ear infections. This procedure involves the use of an otoscope, a device equipped with a light and a magnifying lens, which allows healthcare providers to visualize the ear canal and tympanic membrane (eardrum).
Through otoscopy, healthcare professionals can assess for signs of infection, such as redness, bulging, or fluid behind the eardrum. The following points highlight the significance of otoscopy in the diagnostic process:
Role of Otoscopy in Diagnosing Ear Infections
Otoscopy is essential for an accurate diagnosis of ear infections, as it provides direct visualization of the ear structures. Key aspects include:
- Identification of inflammation: The otoscope allows for the observation of inflammation in the ear canal and eardrum, which are indicative of infection.
- Detection of fluid: Presence of fluid behind the eardrum can be assessed, which often signifies a middle ear infection (otitis media).
- Monitoring chronic conditions: Otoscopy aids in tracking the progression of chronic ear infections and evaluating the effectiveness of ongoing treatments.
In addition to otoscopy, patient history and physical examination play a pivotal role in the diagnostic process. The healthcare provider will gather comprehensive information regarding the patient’s symptoms, which can include ear pain, hearing loss, or discharge.
Importance of Patient History and Physical Examination
The evaluation of a patient’s history and physical examination is crucial for formulating an accurate diagnosis. The following elements are considered:
- Symptom duration and characteristics: Understanding how long symptoms have persisted and their nature can help differentiate between types of ear infections.
- Previous medical history: A record of past ear infections or other related health conditions can provide insights into the current episode.
- Physical examination findings: A thorough examination may reveal additional signs, such as fever or swollen lymph nodes, which can complement the findings from otoscopy.
Overall, the combination of otoscopy, patient history, and physical examination allows healthcare professionals to arrive at an accurate diagnosis, paving the way for effective treatment plans tailored to individual needs. This comprehensive approach is paramount for addressing ear infections and preventing potential complications.
Treatment Options for Ear Infections

Ear infections, though common, require appropriate treatment to ensure a swift recovery and to prevent complications. This section Artikels the various medical treatments available for ear infections, as well as home remedies and self-care techniques that can alleviate symptoms. Understanding these options is crucial for effective management of ear infections.
Medical Treatments for Ear Infections
Medical intervention is often necessary in cases of ear infections, particularly when symptoms are severe or persistent. The primary treatment options include:
- Antibiotics: These are commonly prescribed for bacterial ear infections. It is important to complete the full course of antibiotics as advised by a healthcare professional, even if symptoms improve before finishing the medication.
- Pain relief medications: Over-the-counter analgesics such as acetaminophen or ibuprofen can help alleviate pain and reduce fever associated with ear infections. These medications are particularly beneficial for managing discomfort while waiting for antibiotics to take effect.
- Ear drops: For some patients, especially children, anesthetic ear drops can provide targeted relief from pain. These drops may be prescribed to help manage discomfort.
- Surgery: In chronic cases or when fluid buildup is significant, surgical options such as tympanostomy (the insertion of tubes in the eardrum) may be recommended to facilitate drainage and prevent future infections.
Home Remedies and Self-Care Techniques
In addition to medical treatments, home remedies can play a supportive role in alleviating symptoms associated with ear infections. Patients may consider the following techniques:
- Warm compress: Applying a warm, moist cloth to the affected ear can help soothe pain and discomfort.
- Hydration: Drinking plenty of fluids is essential in managing symptoms and may help thin mucus, which can promote drainage.
- Rest: Adequate rest is crucial for recovery, as the body needs time to heal.
- Elevation: Sleeping with the head elevated can reduce pressure in the ears and improve comfort.
Effectiveness of Antibiotics and Pain Relief Measures
When treating ear infections, both antibiotics and pain relief measures are effective but serve different purposes.
Antibiotics target the underlying bacterial infection, while pain relief medications focus on managing symptoms.
Research indicates that many ear infections, particularly viral ones, may resolve on their own without antibiotics. Therefore, healthcare providers often recommend a wait-and-see approach for mild cases. For more severe infections, antibiotics may be necessary to eliminate the bacteria. Pain relief measures, on the other hand, are consistently effective in managing discomfort and improving quality of life during an ear infection.
Balancing these treatment options is essential for effective management of ear infections, ensuring both symptom relief and recovery from the infection itself.
Prevention Strategies for Ear Infections

Preventing ear infections is essential in safeguarding both children and adults from the discomfort and potential complications associated with these conditions. Various strategies can significantly reduce the risk of developing ear infections, contributing to overall ear health.Several preventive measures can be implemented in daily life to minimize the likelihood of ear infections. These strategies focus on hygiene, environmental factors, and health behaviors that promote ear health.
Preventive Measures
Incorporating preventive measures into daily routines can significantly reduce the risk of ear infections. These strategies include:
- Maintaining good hygiene: Regular handwashing can help prevent the spread of infections that might lead to ear infections.
- Keeping ears dry: Avoiding water entering the ears during bathing or swimming can help prevent infections. Using earplugs or a swim cap can be beneficial.
- Avoiding smoke exposure: Secondhand smoke can irritate the respiratory tract and increase the risk of infections, including ear infections.
- Breastfeeding infants: Breastfeeding for at least the first six months can provide essential antibodies that help protect against infections.
- Encouraging proper nasal hygiene: Teaching children to blow their noses properly can help reduce mucus buildup that may lead to ear infections.
Importance of Vaccinations
Vaccinations play a crucial role in preventing certain illnesses that can lead to ear infections. Immunizations can prevent infections such as influenza and pneumococcal disease, which are known contributors to middle ear infections. Ensuring that children receive their recommended vaccinations on schedule can protect them from complications associated with these diseases.
Lifestyle Changes
Adopting certain lifestyle changes can further aid in the prevention of ear infections. These changes can enhance overall health and immune function, contributing to lower infection rates.
- Encouraging a balanced diet: Consuming a diet rich in vitamins and minerals strengthens the immune system, making the body more resistant to infections.
- Regular physical activity: Engaging in regular exercise can improve overall health and boost the immune system, further reducing the risk of infections.
- Adequate sleep: Ensuring sufficient sleep is vital for maintaining a strong immune system and reducing susceptibility to infections.
- Managing allergies: Properly managing allergies with the help of healthcare professionals can prevent allergy-related ear infections.
- Seeking regular medical check-ups: Regular visits to healthcare providers can help detect and address potential health issues before they lead to ear infections.
When to Seek Medical Attention

Recognizing when to seek medical attention for an ear infection can be crucial for proper treatment and recovery. While many ear infections can be managed at home, certain signs indicate that immediate medical evaluation is necessary. Understanding these red flags and potential complications can help ensure effective care.
Red Flags Indicating Immediate Medical Attention
Certain symptoms warrant prompt medical intervention to prevent complications. If any of the following signs are present, it is essential to consult a healthcare professional without delay:
- Severe ear pain that does not improve with over-the-counter pain relievers.
- Drainage of pus or a significant amount of fluid from the ear.
- Signs of hearing loss, especially sudden changes in hearing ability.
- Fever exceeding 102°F (39°C), particularly in young children.
- Persistent symptoms lasting more than a few days despite home treatment.
- Difficulty balancing or dizziness that interferes with daily activities.
Potential Complications of Untreated Ear Infections
Failing to address an ear infection can lead to several serious complications. These complications may include:
- Chronic Ear Infection: Recurrent infections can occur, leading to long-term issues and potential hearing loss.
- Spread of Infection: The infection may spread to nearby structures, including the mastoid bone (mastoiditis) or even the brain (meningitis).
- Hearing Loss: Prolonged ear infections can result in temporary or permanent hearing impairment due to damage to the ear structures.
Preparation for a Medical Appointment Regarding Ear Infections
Being well-prepared for a medical appointment can facilitate a thorough evaluation and effective treatment plan. Consider the following steps:
- Document Symptoms: Keep a record of symptoms, including their onset and duration, and any changes over time.
- List Medications: Compile a list of all medications and supplements currently being taken, as well as any previous treatments for ear infections.
- Prepare Questions: Write down any questions or concerns regarding the infection, treatment options, and potential side effects.
- Include Medical History: Be ready to discuss relevant family and personal medical history that may impact the diagnosis or treatment.
“Early intervention in ear infections is critical to prevent complications and ensure swift recovery.”
Final Conclusion
In conclusion, recognizing the signs of an ear infection is crucial for ensuring prompt medical attention and preventing complications. By being aware of the symptoms, understanding the risk factors, and knowing when to seek help, individuals can take proactive steps towards maintaining their ear health. Armed with this knowledge, one can navigate the complexities of ear infections more confidently, leading to better outcomes and a healthier life.